1.6%
of the population has BPD
approximately 70%
of people with BPD will make at least one suicide attempt in their lifetimes
between 8 and 10%
of people with BPD will complete suicide
What is Borderline Personality Disorder?
Borderline Personality Disorder (BPD) is a complex mental health condition characterized by intense emotions, unstable relationships, and a deeply rooted fear of abandonment. People with BPD often experience overwhelming feelings and may struggle with their sense of self, leading to emotional ups and downs that can feel difficult to manage. BPD is often misunderstood. It’s not about being “too dramatic” or “manipulative,” it’s about living with a brain wired for intense sensitivity to emotions and relationships. This doesn’t make someone “bad” or “broken,” it means they experience the world deeply.
Common Symptoms of BPD
While everyone’s experience with BPD is unique, some common signs include:.
-Unstable relationships: Shifting between idealizing someone and suddenly feeling disappointed or angry with them (also called “splitting”).
-Intense fear of abandonment: Going to great lengths to avoid real or imagined rejection.
-Extreme emotional swings: Feeling intense emotions that can shift rapidly, from deep sadness to anger to anxiety.
-Chronic feelings of emptiness: A persistent sense of feeling “empty” or disconnected.
-Paranoia or dissociation: Moments of feeling detached from reality, especially during times of stress.
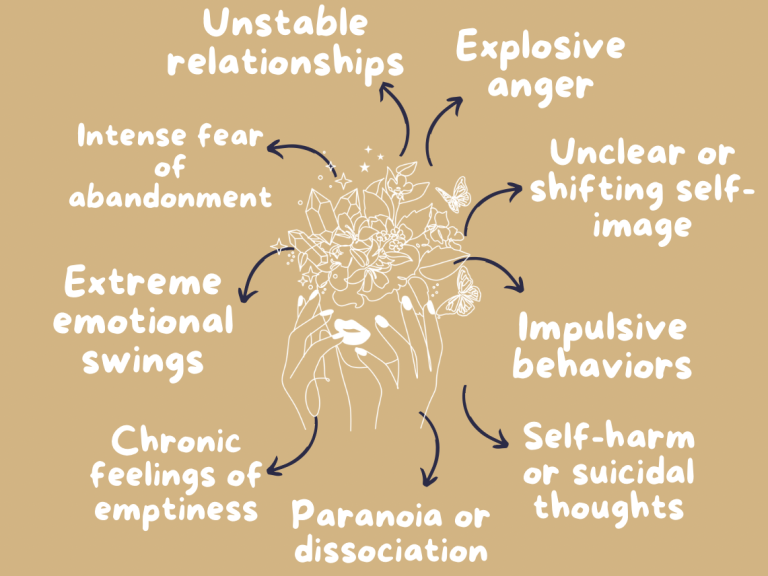
-Explosive anger: Having a hard time controlling your temper, often over small triggers.
-Unclear or shifting self-image: Struggling with identity, feeling unsure of who you are or how you see yourself.
-Impulsive behaviors: Engaging in risky actions, such as reckless driving, spending sprees, or substance use.
-Self-harm or suicidal thoughts: Experiencing intense emotional pain that can lead to self-injury or thoughts of suicide.
Treatments
While there’s no “quick fix,” several evidence-based therapies have been proven effective in treating BPD:
Dialectical Behavior Therapy (DBT)
The gold-standard treatment for BPD, DBT was specifically designed to help people manage intense emotions. DBT empowers individuals to handle emotional surges without destructive behavior, making it a life-changing tool for many.
DBT teaches skills in four key areas:
-Mindfulness: Staying present and grounded in the moment.
-Distress Tolerance: Coping with crisis situations without making things worse.
-Emotion Regulation: Understanding and managing overwhelming emotions.
-Interpersonal Effectiveness: Navigating relationships by setting boundaries and communicating clearly.
Medication
While there’s no specific medication to “cure” BPD, some medications may be prescribed to treat co-occurring symptoms, like:
-Mood stabilizers to reduce mood swings.
-Antidepressants for anxiety or depression.
-Antipsychotics for severe symptoms like paranoia or dissociation.
Medication works best when paired with therapy.
Support Systems
Healing doesn’t happen in isolation. Support from trusted friends, family, and mental health communities plays a huge role in recovery. Many people with BPD also find comfort in:
-Peer support groups: sharing experiences with others who understand.
-Creative outlets: like art, writing, or music to process complex emotions.
-Crisis planning: creating a safety plan with a therapist to navigate tough moments.
©Copyright. All rights reserved.
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.